Make an Appointment
This blog explores the importance of multidisciplinary rehabilitation for stroke patients, with a focus on how physiotherapy, occupational therapy, and speech pathology work together to support recovery.
A stroke can change a person’s life in seconds, disrupting speech, movement, memory, independence, and confidence. Recovery is often complex, requiring not just physical healing but emotional, social, and cognitive rehabilitation as well.
That is why multidisciplinary care is the gold standard in stroke recovery.
Rather than relying on a single provider or therapy, multidisciplinary care brings together a team of professionals, each with their own expertise, who collaborate to support the person as a whole. It ensures that every aspect of recovery is addressed, from re-learning how to walk and talk, to managing fatigue, navigating emotional changes, and rebuilding independence at home.
In this blog, we explain the benefits of a coordinated, multidisciplinary approach to stroke rehabilitation, and how allied health professionals like physiotherapists, occupational therapists, and speech pathologists help stroke survivors rebuild their lives with safety, dignity, and purpose.

Why Is a Multidisciplinary Approach Important in the Management of Stroke Patients?
Stroke survivors often experience a wide range of challenges; including physical weakness, mobility issues, speech or language impairments, swallowing difficulties, emotional regulation problems, cognitive changes, and fatigue. Addressing these complex and overlapping needs requires input from multiple disciplines working in sync.
Core reasons a multidisciplinary approach is vital:
1. Comprehensive recovery
Different specialists target different parts of recovery. For example:
- Physiotherapists restore movement and strength
- Occupational therapists support daily living and routine
- Speech pathologists address communication and swallowing
- Psychologists manage mood and adjustment
- Nurses and case coordinators ensure medical stability and service access
When each professional contributes their expertise, patients receive care that addresses the full picture.
2. Individualised goal setting
The team works with the patient and family to develop meaningful, shared goals. This might include walking to the letterbox, returning to work, or safely eating without assistance.
Each goal is broken down into achievable steps, with each discipline supporting progress from their perspective.
3. Prevention of complications
Multidisciplinary teams monitor for early signs of secondary issues like pressure sores, aspiration pneumonia, falls, depression, or neglect of affected limbs. Collaborative care reduces the risk of complications that can delay or derail progress.
4. Improved communication and handover
Team meetings and shared documentation allow all providers to stay updated on the person’s needs, preferences, and progress—ensuring consistency across therapy sessions.
5. Smoother transitions through the care journey
From hospital discharge to community rehab or NDIS supports, a multidisciplinary team ensures nothing is missed and services are coordinated properly.
Stroke Foundation – Treatment and Recovery
Multidisciplinary care is not just best practice, it is essential for safe, functional, and person-centred recovery.
What Are the Benefits of a Multidisciplinary Approach to Patient Care?
A multidisciplinary team does more than treat a condition, it empowers the person behind the diagnosis.
Key benefits include:
1. Holistic support for the whole person
Stroke recovery is not just about regaining movement. People need help managing anxiety, planning their day, preparing food, and connecting with loved ones. Allied health professionals cover all domains of life, improving quality of care and quality of life.
2. Faster functional progress
When a team works together toward shared goals, outcomes improve. Research shows that stroke survivors in multidisciplinary rehab are more likely to:
- Regain independence in mobility and self-care
- Return to their home instead of long-term care
- Experience shorter rehab stays and lower readmission rates
3. Enhanced safety and reduced risk
Falls, swallowing problems, and medication mismanagement are common risks post-stroke. Having the right team in place minimises these through education, supervision, and adaptive strategies.
4. Family and carer involvement
Carers are an essential part of the recovery journey. Multidisciplinary teams support carers with:
- Education and practical training
- Emotional support and goal setting
- Access to respite and community programs
5. Long-term resilience
Multidisciplinary care fosters sustainable recovery. When people learn how to manage their limitations, use adaptive tools, and maintain healthy routines, they are more likely to thrive in the community over time.
Healthdirect – Stroke Rehabilitation
This model of care improves patient satisfaction, health outcomes, and emotional wellbeing, making it the most effective approach across the continuum of care.

What Benefits Are There for Stroke Victims?
Stroke survivors benefit from multidisciplinary rehabilitation in every aspect of daily life. Here is how it looks across physical, cognitive, and emotional domains:
1. Physical recovery
- Physiotherapists improve strength, posture, gait, and balance
- OTs help with adaptive equipment, fatigue management, and home modifications
- This enables safe transfers, mobility, and independence in personal care
2. Communication and swallowing
- Speech pathologists assist with aphasia, dysarthria, and dysphagia
- Clients can better express needs, understand instructions, and eat safely
- Improved communication boosts confidence and reduces social isolation
3. Emotional adjustment
- Many stroke survivors experience depression, anxiety, grief, or emotional lability
- Psychologists, OTs, and social workers help manage adjustment and emotional regulation
- Support groups and community programs encourage peer connection
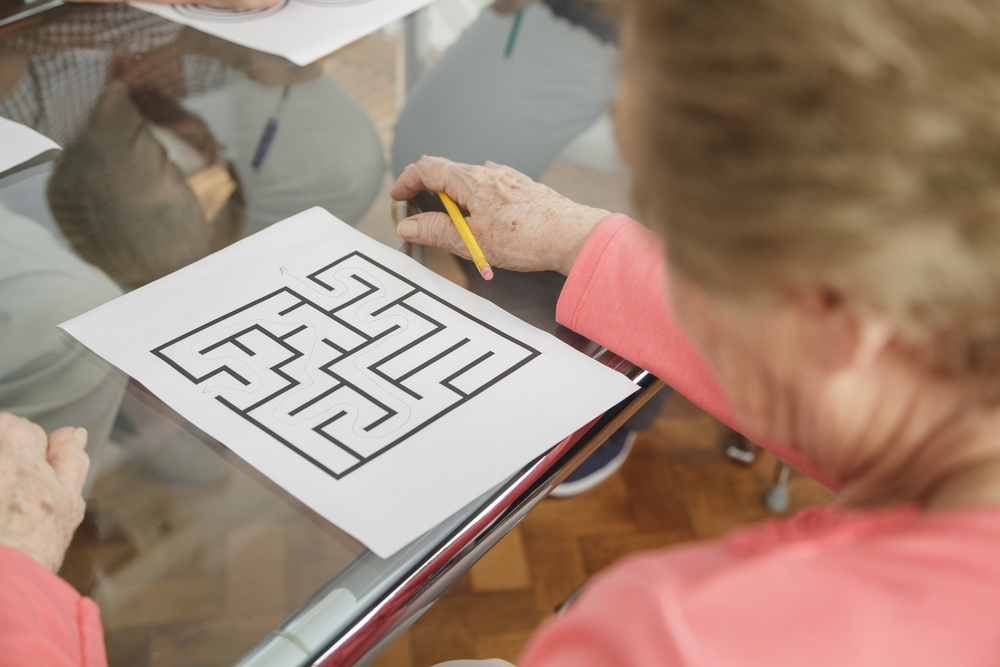
4. Cognitive and perceptual function
- OTs and neuropsychologists address attention, memory, visual-spatial awareness, and executive functioning
- Clients relearn planning, navigation, problem-solving, and safety in their environments
5. Return to meaningful activity
- Whether it is cooking, driving, painting, or working, multidisciplinary teams help clients return to what matters
- Therapists grade tasks, simulate real-life activities, and monitor risk safely
6. Environmental support and advocacy
- Teams work with families, NDIS coordinators, and aged care providers to ensure access to equipment, therapy, transport, and funding
- This improves sustainability of care and reduces hospital readmission
NDIS – Stroke and Neurological Support
Multidisciplinary care transforms “survival” into “recovery”, giving stroke survivors the tools to reclaim independence and identity.

What Is the Most Important Aspect of Stroke Treatment?
The most important aspect of stroke treatment is early, intensive, and coordinated rehabilitation.
While medical treatment stabilises the person, rehabilitation restores function, confidence, and quality of life. Every stroke is different; so every recovery plan must be tailored, flexible, and responsive.
Why early intervention matters:
- The brain has the greatest plasticity in the first few months post-stroke
- Delayed rehab can result in lost mobility, learned helplessness, and unnecessary dependence
- Early rehab helps prevent complications like pressure injuries, joint contractures, and deconditioning
Why intensity and repetition matter:
- Neuroplasticity thrives on repetition and meaningful engagement
- Daily practice of movement, speech, or tasks rewires the brain
- Therapists help ensure rehab is consistent, goal-focused, and motivating
Why collaboration matters:
- No one profession can address all aspects of stroke recovery
- Coordinated care prevents gaps, delays, and conflicting advice
- It also supports carers and reduces strain on the healthcare system
Stroke Foundation – Recovery and Rehabilitation
In summary, the most important aspect of stroke treatment is not just what happens in the hospital, it is what happens in the months and years that follow, and the team that helps guide it.

Frequently Asked Questions (FAQs)
What does a multidisciplinary stroke rehab team include?
Physiotherapists, occupational therapists, speech pathologists, psychologists, dietitians, nurses, and case coordinators often form the core team. Social workers and GPs may also be involved.
How long does stroke rehabilitation take?
This varies depending on the severity of the stroke and individual goals. Some people improve significantly in weeks, while others require long-term support for years.
Can I access stroke rehab through the NDIS?
Yes. If you are eligible, NDIS can fund allied health therapy, assistive technology, home modifications, and community access supports.
Do I need a referral for stroke rehabilitation?
You can access allied health services via a hospital discharge plan, GP referral, My Aged Care, or NDIS. You can also self-refer to a provider like Physio Inq.
What if I live in a rural or remote area?
Mobile and telehealth services can bring rehab to your home. Many providers offer flexible options to ensure continuity of care.

Final thoughts
Stroke recovery is complex, but no one should face it alone. A multidisciplinary team ensures that every aspect of care is covered, with compassion, coordination, and clinical expertise.
Whether you are a stroke survivor, a carer, or a health professional, understanding the value of collaborative rehabilitation can change the recovery journey. With the right team and support, recovery is not only possible, it can be empowering.
Next Steps
Call 1300 731 733 or book online to build a multidisciplinary recovery plan with our experienced team of physiotherapists, occupational therapists, and speech pathologists.
You can also:
- Explore our Neurological Rehabilitation Services
- Read our guide to in-home stroke support
- Share this article with your care team or case manager
- Request a multidisciplinary team meeting or NDIS review
- Ask about mobile or telehealth stroke therapy near you

Date Published: Tuesday, July 8, 2025
Locate a Aged Care Exercise Physiology
Service Near me
Get the experience & convinence you deserve to support your or a loved one's allied health needs.
Our Aged Care Exercise Physiology team are currently serving & taking appointments in the following states and regions in Australia:
Need to get into direct contact with ur Client Services team? We're all ears. Call our team directly on 1300 731 733






